Children’s National in the News: 2023

Explore some of the notable medical advancements and stories of bravery that defined 2023, showcasing the steadfast commitment of healthcare professionals at Children’s National Hospital and the resilient spirit of the children they support. Delve into our 2023 news highlights for more.
1. COVID during pregnancy dramatically increases the risk of complications and maternal death, large new study finds
According to a study published in British Medical Journal Global Health, women who get COVID during pregnancy are nearly eight times more likely to die and face a significantly elevated risk of ICU admission and pneumonia. Sarah Mulkey, M.D., prenatal-neonatologist neurologist, discussed findings based on her work with pregnant women and their babies.
(Fortune)
2. Rest isn’t necessarily best for concussion recovery in children, study says
A study led by Christopher Vaughan, Psy.D., pediatric neuropsychologist, suggests that — despite what many people may presume — getting kids back to school quickly is the best way to boost their chance for a rapid recovery after a concussion.
(CNN)
3. Pediatric hospital beds are in high demand for ailing children. Here’s why
David Wessel, M.D., executive vice president, chief medical officer and physician-in-chief, explained that one reason parents were still having trouble getting their children beds in a pediatric hospital or a pediatric unit after the fall 2022 respiratory surge is that pediatric hospitals are paid less by insurance.
(CNN)
4. Anisha Abraham details impact of social media use on children: ‘True mental health crisis’
Anisha Abraham, M.D., M.P.H., chief of the Division of Adolescent and Young Adult Medicine, joined America’s Newsroom to discuss the impact social media access has had on children’s mental health.
(FOX News)
5. Saving Antonio: Can a renowned hospital keep a boy from being shot again?
After 13-year-old Antonio was nearly killed outside his mom’s apartment, Children’s National Hospital went beyond treating his bullet wounds. Read how our Youth Violence Intervention Program team supported him and his family during his recovery.
(The Washington Post)
6. Formerly conjoined twins reunite with doctors who separated them
Erin and Jade Buckles underwent a successful separation at Children’s National Hospital. Nearly 20 years later they returned to meet with some of the medical staff who helped make it happen.
(Good Morning America)
7. Asthma mortality rates differ by location, race/ethnicity, age
Shilpa Patel, M.D., M.P.H., medical director of the Children’s National IMPACT DC Asthma Clinic, weighed in on a letter published in Annals of Allergy, Asthma & Immunology, asserting that the disparities in mortality due to asthma in the United States vary based on whether they occurred in a hospital, ethnicity or race and age of the patient.
(Healio)
8. How one Afghan family made the perilous journey across the U.S.-Mexico border
After one family embarked on a perilous journey from Afghanistan through Mexico to the U.S.-Mexico border, they eventually secured entry to the U.S. where Karen Smith, M.D., medical director of Global Services, aided the family’s transition and provided their daughter with necessary immediate medical treatment.
(NPR)
9. When a child is shot, doctors must heal more than just bullet holes
With the number of young people shot by guns on the rise in the U.S., providers and staff at Children’s National Hospital are trying to break the cycle of violence. But it’s not just the physical wounds though that need treating: young victims may also need help getting back on the right track — whether that means enrolling in school, finding a new group of friends or getting a job.
(BBC News)
10. This 6-year-old is a pioneer in the quest to treat a deadly brain tumor
Callie, a 6-year-old diagnosed with diffuse intrinsic pontine glioma, was treated with low-intensity focused ultrasound (LIFU) at Children’s National Hospital and is the second child in the world to receive this treatment for a brain tumor. LIFU is an emerging technology that experts like Hasan Syed, M.D., and Adrianna Fonseca, M.D., are trialing to treat this fatal childhood brain tumor.
(The Washington Post)
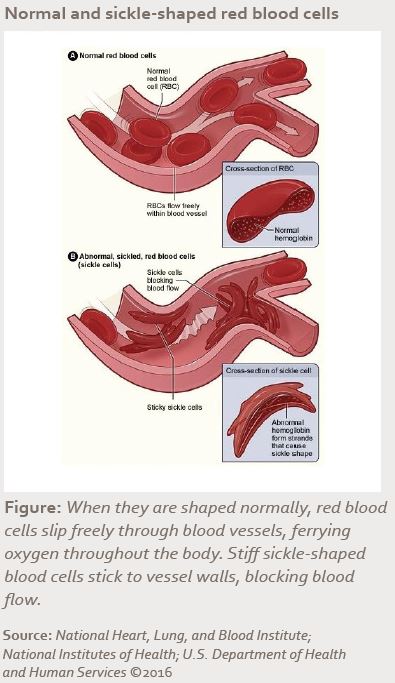
11. F.D.A. approves sickle cell treatments, including one that uses CRISPR
The FDA approved a new genetic therapy, giving people with sickle cell disease new opportunities to eliminate their symptoms. David Jacobsohn, M.B.A., M.D., confirmed that Children’s National Hospital is one of the authorized treatment centers and talked about giving priority to the sickest patients if they are on Vertex’s list.
(The New York Times)
12. 6-year-old fulfils wish to dance in the Nutcracker
After the potential need for open-heart surgery threatened Caroline’s Nutcracker performance, Manan Desai, M.D., a cardiac surgeon, figured out a less invasive procedure to help reduce her recovery time so she could perform in time for the holidays.
(Good Morning America)